Table of Contents
ToggleDiabetes and your eyes: What you need to know

Diabetes is a chronic condition that affects how your body regulates blood sugar (glucose). While most people know that diabetes can impact the heart, kidneys, and nerves, its effects on the eyes are often underestimated. High blood sugar can damage delicate eye structures over time, leading to vision problems — and in severe cases, blindness.
Understanding these risks is the first step in protecting your sight. This blog explains how diabetes affects the eyes, the warning signs to watch for, and practical steps you can take to maintain healthy vision.
How does diabetes affect your eyes?
Consistently high blood sugar levels can damage small blood vessels and nerves in the eye. Over time, this damage can lead to several eye conditions, including:
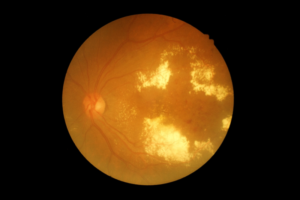
Diabetic retinopathy

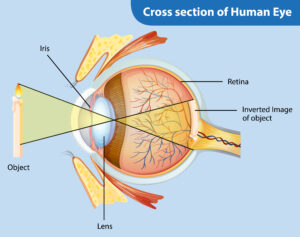
- Diabetic retinopathy is one of the most common eye complications caused by diabetes. It occurs when high blood sugar levels damage the tiny blood vessels in the retina, the light-sensitive tissue at the back of the eye. In the early stages, there may be no noticeable symptoms, making regular eye check-ups essential. As the disease progresses, new abnormal blood vessels may grow and leak fluid or blood into the eye. This can cause blurred vision, the appearance of dark spots (floaters), and in severe cases, significant vision loss or blindness. Early detection and treatment are crucial to prevent long-term damage.
2. Diabetic Macular Oedema (DMO)
- Diabetic macular oedema is a complication of diabetic retinopathy where fluid leaks into the macula, the central part of the retina responsible for sharp, detailed vision. The swelling in the macula makes it difficult to see fine details, read clearly, or recognise faces. People with DMO may notice that their vision becomes blurry or distorted, especially in the central part of their sight. Since the macula is critical for tasks like driving, reading, and recognising objects, untreated DMO can significantly affect daily life.
3. Cataracts

- A cataract is the clouding of the eye’s natural lens, which normally helps focus light onto the retina. While cataracts are common with aging, people with diabetes are at a higher risk of developing them earlier and at a faster rate. This happens because high blood sugar levels can cause changes in the lens proteins, leading to cloudiness. Symptoms include blurry vision, dim or faded colours, difficulty seeing at night, and increased sensitivity to glare. Cataract surgery is often required to restore clear vision.
4. Glaucoma

- Glaucoma is a group of eye diseases that damage the optic nerve, usually due to increased pressure inside the eye. People with diabetes are at a higher risk of developing glaucoma compared to the general population. This increased eye pressure can slowly damage the optic nerve, often without early warning signs. In most cases, glaucoma develops gradually and is only noticeable once significant vision has been lost. Symptoms may include patchy blind spots in the peripheral vision and, in advanced cases, tunnel vision. Regular eye exams are essential because early treatment can slow or prevent further damage.
Early warning signs to watch for
Diabetes-related eye disease can progress silently. Seek an eye examination promptly if you notice:
- Blurred or fluctuating vision.
- Dark spots or “floaters” in your sight.
- Poor night vision.
- Eye pain or pressure.
- Sudden loss of vision in one or both eyes.
How to protect your vision with diabetes?
Good diabetes management and regular eye check-ups are key to preventing vision loss. Here is what we recommend:
Schedule regular eye exams
- Even if your vision seems fine, have a comprehensive dilated eye exam at least once a year.
Control vascular risk factors
Keeping blood sugar, blood pressure, and cholesterol under control is essential to
protect the eyes and overall health.
- High blood sugar can damage the tiny blood vessels in the retina, leading to leakage, swelling, or abnormal vessel growth that causes diabetic retinopathy and vision loss.
- High blood pressure increases strain on retinal vessels, raising the risk of glaucoma, optic nerve damage, and bleeding.
- High cholesterol can block blood flow in the retina and cause sudden vision problems or macular degeneration.
By keeping all three within healthy ranges, by complying with management prescribed by your treating doctor, and attending regular checkups, individuals can significantly reduce their risk of eye damage and preserve long-term vision.
Quit smoking
- Smoking increases the risk of diabetic eye disease progression.
- Smoking increases the risk of diabetic eye disease progression.
Maintain a healthy lifestyle
- Balanced diet, regular exercise, and proper hydration support both overall and eye health.
- Balanced diet, regular exercise, and proper hydration support both overall and eye health.
Seek prompt treatment
- If your ophthalmologist detects early signs of diabetic eye disease, timely treatment such as laser therapy, eye injections, or surgery can help preserve vision.
Treatment options at Clarity Eye Surgeons
Our clinic provides advanced treatments for diabetes-related eye problems, including:
- Intravitreal eye injections for macular oedema.
- Laser therapy for diabetic retinopathy.
- Cataract surgery for vision clouding.
- Glaucoma management using medications or surgery.
We combine modern technology with personalised care to help you maintain healthy eyesight for life.
Conclusion
Diabetes does not have to lead to vision loss — but early detection and consistent care are essential. At Clarity Eye Surgeons, we are committed to helping patients in Canberra and surrounding areas protect their sight through expert diagnosis, advanced treatments, and compassionate care.
Book your diabetic eye examination today and take the first step toward safeguarding your vision.
Author bio
Dr Parth Shah is a director and principal ophthalmologist in Canberra at Clarity Eye Surgeons. With extensive training and experience, he is renowned for his expertise in the field. Dr Shah is dedicated not only to performing successful surgeries but also to patient education. His compassionate approach, combined with technical proficiency, has earned him the trust and gratitude of countless patients. He is a true advocate for eye health and a trusted name in the Canberra ophthalmology community.
FAQs
Yes. While many diabetic eye conditions progress slowly, sudden changes — like blurred vision or loss of sight — may indicate a complication such as vitreous haemorrhage or retinal detachment, requiring urgent care.
Some early changes can be improved with good blood sugar control, but advanced damage (like severe retinopathy) often causes permanent vision loss. Prompt treatment can slow or stop progression.
Ideally, within the first few months of diagnosis, and then annually, or more frequently if recommended by your eye specialist.
No. Good blood sugar management, regular check-ups, and a healthy lifestyle significantly reduce the risk.
Yes, although it is less likely and usually less severe. Long-term diabetes still increases the risk, so routine monitoring is important.
No, most people do not feel pain. That is why it can go unnoticed until vision is affected — making regular eye exams essential.
Yes, damage to the retina can sometimes reduce colour perception, especially in advanced stages.
In general, foods rich in omega-3 fatty acids, antioxidants (like lutein and zeaxanthin), and vitamins C and E can support retinal health.
Other blogs related to Eye Conditions
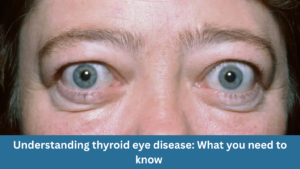
Understanding thyroid eye disease: What you need to know
Understanding thyroid eye disease: What you need to know At Clarity Eye Surgeons in Canberra, our team of skilled ophthalmologists in Canberra brings years of
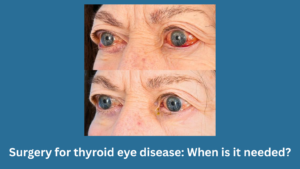
Surgery for thyroid eye disease: When is it needed?
Surgery for thyroid eye disease: When is it needed? At Clarity Eye Surgeons in Canberra, our team of experienced ophthalmologists, led by Dr Parth Shah,

Pterygium surgery: What to expect before, during, and after?
Pterygium surgery: What to expect before, during, and after? At Clarity Eye Surgeons in Canberra, patients receive expert care led by Dr Parth Shah, a

Living with thyroid eye disease: Treatment options explained
Living with thyroid eye disease: Treatment options explained At Clarity Eye Surgeons in Canberra, our team of highly qualified ophthalmologists has extensive experience diagnosing and
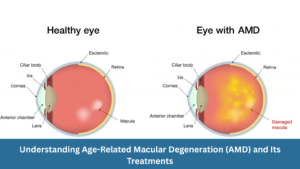
Understanding Age-Related Macular Degeneration (AMD) and Its Treatments
Understanding Age-Related Macular Degeneration (AMD) and Its Treatments At Clarity Eye Surgeons, we bring decades of ophthalmic expertise and advanced surgical experience to help Canberra

Diabetic eye disease: How to prevent vision loss?
Diabetic eye disease: How to prevent vision loss? What is diabetic eye disease? Diabetic eye disease refers to a group of eye conditions that can

Common vision problems in children and how to spot them early
Common vision problems in children and how to spot them early At Clarity Eye Surgeons in Canberra, our team of highly experienced paediatric ophthalmologists and

Double vision in children: What parents should know
Double vision in children: What parents should know Double vision, medically called diplopia, occurs when a child sees two images of a single object instead

Glaucoma: What it is, Symptoms, Causes, Types & Treatment
Glaucoma: What it is, Symptoms, Causes, Types & Treatment Glaucoma is often called the “silent thief of sight” because it can damage your vision gradually,

Living with wet macular degeneration: Treatment options and lifestyle tips
Living with wet macular degeneration: Treatment options and lifestyle tips Wet macular degeneration, also known as neovascular age-related macular degeneration (AMD), is a chronic eye

Retinal detachment: Early signs you should never ignore
Retinal detachment: Early signs you should never ignore Your eyes are extraordinary organs that allow you to experience the world in vivid colour, detail, and

Vitrectomy: What you need to know
Vitrectomy: What you need to know Vitrectomy is a specialised eye surgery performed to treat a range of disorders affecting the retina and vitreous —

Diabetes and your eyes: What you need to know
Diabetes and your eyes: What you need to know Diabetes is a chronic condition that affects how your body regulates blood sugar (glucose). While most

Nystagmus: Symptoms, Causes, and Treatments
Nystagmus: Symptoms, Causes, and Treatments Nystagmus is a condition in which the eyes make uncontrolled, repetitive movements. These movements can be slow or fast, side-to-side

What to know about blurry vision and diabetes?
What to know about blurry vision and diabetes? Blurry vision is a common and often early symptom of diabetes. If you or someone you know
Chalazion surgery: When is it necessary and What to expect
Chalazion surgery: When is it necessary and What to expect A chalazion is a common eyelid condition that can lead to discomfort, swelling, and cosmetic

Are prescription glasses effective for treating lazy eye?
Are prescription glasses effective for treating lazy eye? Lazy eye, also known as amblyopia, is a common vision problem in children, affecting a small percentage

Dry Eye Syndrome: Symptoms, Causes & Treatment
Dry Eye Syndrome: Symptoms, Causes & Treatment Do your eyes often feel dry, irritated, or fatigued? You might be experiencing Dry Eye Syndrome (DES)—a common

The Relationship Between Allergies and Eye Health in Children
The Relationship Between Allergies and Eye Health in Children Allergies are a prevalent concern among children and can significantly impact their quality of life. While

Understanding Astigmatism: Symptoms, Causes, Diagnosis, Treatment Options & Prevention
Understanding Astigmatism: Symptoms, Causes, Diagnosis, Treatment Options & Prevention What is Astigmatism? Astigmatism is a common eye condition that affects how your eye focuses light.
Understanding Retinal Detachment: Causes, Symptoms, Diagnosis and Treatment
Understanding Retinal Detachment: Causes, Symptoms, Diagnosis and Treatment As the principal ophthalmologist at Clarity Eye Surgeons, Dr Parth Shah is passionate about educating our patients
