Table of Contents
ToggleSurgery for thyroid eye disease: When is it needed?
At Clarity Eye Surgeons in Canberra, our team of experienced ophthalmologists, led by Dr Parth Shah, specialises in diagnosing and treating complex eye conditions, including thyroid eye disease (TED). With 10 years of expertise in managing this condition, we combine evidence-based techniques and advanced surgical care to restore both eye health and appearance. Our commitment to precision, safety, and patient-centred care has earned us the trust of numerous patients seeking effective solutions for thyroid-related eye problems.
What is thyroid eye disease and how does it affect the eyes?
Thyroid eye disease is an autoimmune condition where the body’s immune system mistakenly attacks the tissues around the eyes, causing inflammation, swelling, and bulging of the eyeballs. It most commonly occurs in people with Graves’ disease, but it can also appear in those with other thyroid imbalances.
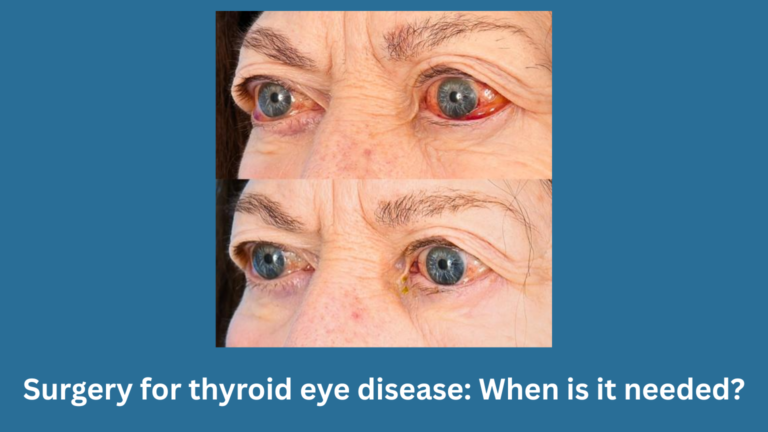
In early stages, symptoms may include redness, dryness, double vision, and puffiness around the eyes. As the condition progresses, it may lead to vision changes, eyelid retraction, or difficulty closing the eyes fully. Severe cases can even threaten sight due to pressure on the optic nerve.
When is surgery needed for thyroid eye disease?
Surgery for thyroid eye disease is usually considered when the active (inflammatory) phase of the disease has settled, and symptoms remain that cannot be corrected with medical treatment alone.
It is typically needed when:
- Vision is threatened due to optic nerve compression.
- The eyes are bulging (proptosis) severely, causing discomfort or exposure.
- The eyelids are retracted, making it difficult to close the eyes or blink properly.
- Double vision (diplopia) persists despite medical management.
- There is noticeable facial asymmetry or cosmetic concern impacting confidence.
Doctors usually wait until the disease has been stable for at least 6 to 12 months before recommending surgery, as operating too early may lead to unpredictable results.
What are the types of surgery for thyroid eye disease?
Treatment for thyroid eye disease is often staged and depends on the specific symptoms. Common surgical options include:
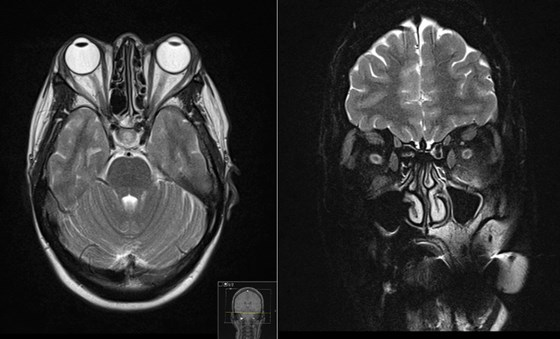
- Orbital decompression surgery – this procedure creates more space in the eye socket by removing bone or fat, helping the eyes move back to a more natural position and relieving pressure on the optic nerve.
- Strabismus (eye muscle) surgery – performed to correct double vision by adjusting the position or length of the eye muscles.
- Eyelid surgery – helps to correct eyelid retraction or puffiness, improving both function and appearance.
These surgeries may be done individually or in sequence, depending on the severity and combination of symptoms.
How long does recovery take after thyroid eye surgery?
Recovery time varies depending on the type of surgery performed. Most patients can resume normal activities within 1 to 2 weeks, but full healing may take several months. Swelling and bruising around the eyes usually improve within a few weeks.
Patients are advised to avoid strenuous activities and follow all post-operative care instructions. Regular follow-ups with the ophthalmologist ensure the eyes heal properly and that vision remains stable.
What results can you expect after surgery?
The goal of surgery is to restore eye comfort, protect vision, and improve appearance. Many patients experience:
- Significant reduction in eye bulging.
- Improved ability to close eyelids.
- Relief from double vision.
- Enhanced facial symmetry and confidence.
While surgery offers long-lasting benefits, results depend on the severity of the disease and the timing of intervention. Combining surgery with good thyroid control and healthy lifestyle choices ensures better long-term outcomes.
How can you prevent thyroid eye disease from worsening?

Although thyroid eye disease cannot always be prevented, certain steps can help reduce its severity:
- Maintain stable thyroid hormone levels with regular medical follow-ups.
- Stop smoking, as it significantly worsens symptoms.
- Wear sunglasses to protect from wind and light sensitivity.
- Use lubricating eye drops to reduce dryness.
- Sleep with your head elevated to minimise swelling.
Early diagnosis and coordinated care between an endocrinologist and an eye specialist are key to managing the condition effectively.
When should you visit an eye specialist?
If you experience eye bulging, double vision, or persistent irritation along with thyroid problems, it is essential to consult an ophthalmologist experienced in thyroid eye disease. Early evaluation helps in preventing complications and planning the right treatment pathway.
Conclusion
At Clarity Eye Surgeons, we provide comprehensive evaluation and personalised surgical care for patients with thyroid eye disease. Led by Dr Parth Shah, our team combines surgical precision, compassionate care, and advanced technology to help patients regain comfort, confidence, and vision clarity.
If you suspect thyroid eye disease or are considering surgery, book an appointment at Clarity Eye Surgeons in Canberra for expert guidance and trusted care.
Author bio
Dr Parth Shah is a director and principal ophthalmologist at Clarity Eye Surgeons in Canberra. With extensive training and experience, he is renowned for his expertise in the field. Dr Shah is dedicated not only to performing successful surgeries but also to patient education. His compassionate approach, combined with technical proficiency, has earned him the trust and gratitude of countless patients. He is a true advocate for eye health and a trusted name in the Canberra ophthalmology community.
FAQs
Thyroid eye disease can sometimes improve on its own once thyroid levels are stabilised, especially in mild cases. However, in many patients, the changes around the eyes do not completely resolve and may require medical or surgical treatment to correct persistent symptoms or cosmetic concerns.
Most thyroid eye surgeries are performed under general anaesthesia, so you would not feel pain during the procedure. Some mild discomfort, swelling, or tightness around the eyes is common after surgery but can be managed effectively with prescribed pain relief and post-operative care.
Yes. While it is more common in those with overactive thyroid (Graves’ disease), thyroid eye disease can also occur in people with normal or even low thyroid hormone levels. This happens because the condition is driven by an autoimmune response rather than just thyroid hormone imbalance.
Most specialists recommend waiting until the disease has been inactive and stable for at least six to twelve months before proceeding with surgery. This ensures that inflammation has settled and that surgical results will be more predictable and lasting.
Once the disease becomes inactive, it usually does not flare up again. However, in rare cases, especially if thyroid hormone levels become unstable or if the patient smokes, there may be a recurrence of symptoms. Maintaining stable thyroid function and a healthy lifestyle helps prevent relapse.
Yes, in many cases, both eyes can be operated on during the same procedure. However, the decision depends on the severity of the disease in each eye and the type of surgery being performed. Your ophthalmologist will assess which approach will provide the safest and most effective outcome.
Yes. During the active phase, treatments may include corticosteroids, immunosuppressive medications, or targeted biologic therapies to reduce inflammation. Lubricating drops and prism glasses may also help with dryness or double vision. Surgery is considered when these measures are not sufficient.
Other blogs related to eye conditions
Understanding thyroid eye disease: What you need to know
Understanding thyroid eye disease: What you need to know At Clarity Eye Surgeons in Canberra, our team of skilled ophthalmologists in Canberra brings years of
Surgery for thyroid eye disease: When is it needed?
Surgery for thyroid eye disease: When is it needed? At Clarity Eye Surgeons in Canberra, our team of experienced ophthalmologists, led by Dr Parth Shah,

Pterygium surgery: What to expect before, during, and after?
Pterygium surgery: What to expect before, during, and after? At Clarity Eye Surgeons in Canberra, patients receive expert care led by Dr Parth Shah, a

Living with thyroid eye disease: Treatment options explained
Living with thyroid eye disease: Treatment options explained At Clarity Eye Surgeons in Canberra, our team of highly qualified ophthalmologists has extensive experience diagnosing and
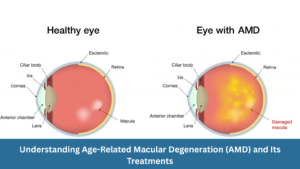
Understanding Age-Related Macular Degeneration (AMD) and Its Treatments
Understanding Age-Related Macular Degeneration (AMD) and Its Treatments At Clarity Eye Surgeons, we bring decades of ophthalmic expertise and advanced surgical experience to help Canberra

Diabetic eye disease: How to prevent vision loss?
Diabetic eye disease: How to prevent vision loss? What is diabetic eye disease? Diabetic eye disease refers to a group of eye conditions that can

Common vision problems in children and how to spot them early
Common vision problems in children and how to spot them early At Clarity Eye Surgeons in Canberra, our team of highly experienced paediatric ophthalmologists and

Double vision in children: What parents should know
Double vision in children: What parents should know Double vision, medically called diplopia, occurs when a child sees two images of a single object instead

Glaucoma: What it is, Symptoms, Causes, Types & Treatment
Glaucoma: What it is, Symptoms, Causes, Types & Treatment Glaucoma is often called the “silent thief of sight” because it can damage your vision gradually,

Living with wet macular degeneration: Treatment options and lifestyle tips
Living with wet macular degeneration: Treatment options and lifestyle tips Wet macular degeneration, also known as neovascular age-related macular degeneration (AMD), is a chronic eye

Retinal detachment: Early signs you should never ignore
Retinal detachment: Early signs you should never ignore Your eyes are extraordinary organs that allow you to experience the world in vivid colour, detail, and

Vitrectomy: What you need to know
Vitrectomy: What you need to know Vitrectomy is a specialised eye surgery performed to treat a range of disorders affecting the retina and vitreous —

Diabetes and your eyes: What you need to know
Diabetes and your eyes: What you need to know Diabetes is a chronic condition that affects how your body regulates blood sugar (glucose). While most

Nystagmus: Symptoms, Causes, and Treatments
Nystagmus: Symptoms, Causes, and Treatments Nystagmus is a condition in which the eyes make uncontrolled, repetitive movements. These movements can be slow or fast, side-to-side

What to know about blurry vision and diabetes?
What to know about blurry vision and diabetes? Blurry vision is a common and often early symptom of diabetes. If you or someone you know
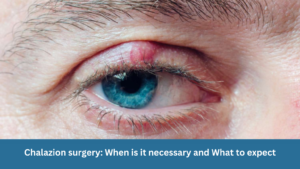
Chalazion surgery: When is it necessary and What to expect
Chalazion surgery: When is it necessary and What to expect A chalazion is a common eyelid condition that can lead to discomfort, swelling, and cosmetic

Are prescription glasses effective for treating lazy eye?
Are prescription glasses effective for treating lazy eye? Lazy eye, also known as amblyopia, is a common vision problem in children, affecting a small percentage

Dry Eye Syndrome: Symptoms, Causes & Treatment
Dry Eye Syndrome: Symptoms, Causes & Treatment Do your eyes often feel dry, irritated, or fatigued? You might be experiencing Dry Eye Syndrome (DES)—a common

The Relationship Between Allergies and Eye Health in Children
The Relationship Between Allergies and Eye Health in Children Allergies are a prevalent concern among children and can significantly impact their quality of life. While

Understanding Astigmatism: Symptoms, Causes, Diagnosis, Treatment Options & Prevention
Understanding Astigmatism: Symptoms, Causes, Diagnosis, Treatment Options & Prevention What is Astigmatism? Astigmatism is a common eye condition that affects how your eye focuses light.
Understanding Retinal Detachment: Causes, Symptoms, Diagnosis and Treatment
Understanding Retinal Detachment: Causes, Symptoms, Diagnosis and Treatment As the principal ophthalmologist at Clarity Eye Surgeons, Dr Parth Shah is passionate about educating our patients
