Table of Contents
ToggleLiving with thyroid eye disease: Treatment options explained

At Clarity Eye Surgeons in Canberra, our team of highly qualified ophthalmologists has extensive experience diagnosing and treating thyroid eye disease (TED). Combining advanced medical knowledge, 10 years of surgical expertise, and a patient-centred approach, Dr Parth Shah delivers comprehensive care for individuals affected by this complex condition.
Our specialists are recognised for their skill, ensuring accurate assessment, personalised treatment planning, and long-term visual protection. We are dedicated to restoring not only eye health but also confidence and comfort for every patient living with thyroid-related eye changes.
What is thyroid eye disease and how does it affect your eyes and vision?
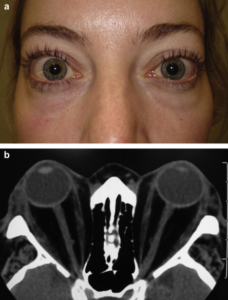
Thyroid eye disease (TED)—also known as Graves’ orbitopathy or thyroid-associated ophthalmopathy—is an autoimmune condition where the immune system mistakenly attacks the tissues around the eyes. This leads to inflammation, swelling, and tissue remodelling behind the eye.
The disease often develops in people with an overactive thyroid (hyperthyroidism) due to Graves’ disease, but it can also occur in those with normal or low thyroid function.
Common symptoms include:
- Eye bulging or prominence. (proptosis)
- Redness, swelling, or puffiness around the eyes.
- Grittiness or dryness.
- Double vision. (diplopia)
- Difficulty closing the eyes.
- Pain or pressure behind the eyes.
- Sensitivity to light.
In severe cases, TED can lead to compression of the optic nerve, causing blurred or reduced vision. Early detection and proper management are vital to prevent long-term visual damage.
What causes thyroid eye disease to develop?
Thyroid eye disease is caused by an abnormal autoimmune response. The immune system produces antibodies that target the tissues surrounding the eyes—especially the muscles and fat within the eye socket (orbit).
Several factors can increase the risk of developing or worsening TED:
- Uncontrolled thyroid hormone levels. (hyperthyroidism or hypothyroidism)
- Smoking, which greatly increases disease severity and risk of progression.
- Family history of autoimmune thyroid disorders.
- Gender and age, as the condition is more common in middle-aged women.
- Radioactive iodine therapy, which can sometimes trigger or worsen TED in certain patients.
How is thyroid eye disease diagnosed?
At Clarity Eye Surgeons in Canberra, our diagnosis process involves a comprehensive eye assessment to evaluate disease activity, eye movement, and visual function.
Diagnostic steps may include:
- Detailed eye examination: Assessing eye movement, eyelid position, corneal health, and optic nerve function.
- Thyroid function tests: Measuring levels of thyroid hormones (T3, T4, TSH) and antibodies to determine underlying thyroid imbalance.
- Imaging tests: MRI or CT scans of the orbits help visualise inflammation, muscle enlargement, and pressure on the optic nerve.
Accurate diagnosis helps us determine whether the disease is in its active (inflammatory) or inactive (stable) phase, which is crucial for choosing the right treatment.
What are the treatment options for thyroid eye disease?
Treatment for thyroid eye disease is tailored to the stage, severity, and symptoms of the condition. The goal is to control inflammation, relieve discomfort, and protect vision.
1. Medical management for mild cases
In the early or mild stage, management may include:
- Lubricating eye drops and gels to relieve dryness and irritation.
- Cold compresses to reduce swelling and redness.
- Sleeping with head elevated to minimise overnight puffiness.
- Smoking cessation, as quitting smoking significantly improves treatment outcomes.
- Thyroid hormone control under guidance from an endocrinologist.
2. Corticosteroid therapy
For active inflammation, steroid treatment (oral or intravenous) can effectively reduce swelling and discomfort. This helps protect the optic nerve and prevent further tissue damage.
3. Immunosuppressive and targeted biological therapy
For patients with moderate to severe TED, newer biological agents can help modulate the immune response:
- Teprotumumab, an FDA-approved targeted therapy, helps reduce inflammation and eye bulging.
- Rituximab or mycophenolate mofetil may be considered for specific immune-mediated cases.
These treatments are used under specialist supervision, ensuring safety and effectiveness.
4. Orbital radiotherapy
Low-dose orbital radiotherapy can help control inflammation and reduce muscle swelling in selected patients. It is often combined with corticosteroids for improved results.
5. Surgical treatment for inactive or stable disease
Once the active inflammation subsides, surgery may be considered to correct residual effects such as eye bulging, eyelid retraction, or double vision.
Common surgical options include:
- Orbital decompression surgery – to create more space for the swollen tissues and reduce eye bulging.
- Strabismus surgery – to realign the eyes and correct double vision.
- Eyelid surgery – to restore natural eyelid position and improve eye protection.
When should you consult an eye specialist for thyroid eye disease?
You should see a specialist ophthalmologist or oculoplastic surgeon if you experience any of the following:
- Persistent eye swelling or bulging.
- Pain, pressure, or tightness around the eyes.
- Double vision or difficulty focusing.
- Changes in eye appearance or movement.
- Reduced or blurry vision.
Early referral and treatment greatly improve the likelihood of preserving vision and achieving better cosmetic and functional outcomes.
How do Clarity Eye Surgeons manage thyroid eye disease?
At Clarity Eye Surgeons, we provide a comprehensive and multidisciplinary approach to treating thyroid eye disease. Our ophthalmologists collaborate closely with endocrinologists to stabilise thyroid hormone levels while addressing eye symptoms effectively.
Our approach includes:
- Thorough evaluation and imaging to assess orbital inflammation and eye alignment.
- Individualised treatment planning, from medical therapy to advanced surgical correction.
- Modern surgical techniques for orbital decompression and eyelid repair to enhance both vision and appearance.
- Long-term follow-up care to monitor disease stability and prevent recurrence.
Our mission is to help patients restore eye comfort, function, and confidence through safe, evidence-based care.
Can thyroid eye disease be cured completely?
While thyroid eye disease cannot always be completely cured, it can be effectively controlled and its impact reduced. Once the disease becomes inactive, symptoms often stabilise or improve with appropriate medical and surgical treatment.
With expert care, most patients experience significant improvement in both visual function and cosmetic appearance, allowing them to return to daily life with comfort and confidence.
Conclusion
Living with thyroid eye disease can be physically and emotionally challenging, but you do not have to face it alone. At Clarity Eye Surgeons, we combine clinical excellence, compassion, and modern technology to deliver the best outcomes for our patients.
If you are experiencing symptoms of thyroid eye disease, early evaluation is key. Contact Clarity Eye Surgeons today to schedule a consultation and take the first step towards protecting your vision and restoring your quality of life.
Author bio
Dr Parth Shah is a director and principal ophthalmologist at Clarity Eye Surgeons in Canberra. With extensive training and experience, he is renowned for his expertise in the field. Dr Shah is dedicated not only to performing successful surgeries but also to patient education. His compassionate approach, combined with technical proficiency, has earned him the trust and gratitude of countless patients. He is a true advocate for eye health and a trusted name in the Canberra ophthalmology community.
FAQs
Thyroid eye disease typically has an active phase lasting between six months and two years. During this period, inflammation and changes in the eye tissues occur. After the active phase, the condition usually becomes stable or inactive, though some effects may remain and can be managed surgically if needed.
Yes. Although TED commonly affects both eyes, it can sometimes appear asymmetrically—where one eye is more affected than the other, or occasionally, only one eye shows symptoms. This makes regular specialist monitoring crucial for accurate assessment.
Stress itself does not directly cause thyroid eye disease, but it can worsen autoimmune activity and thyroid hormone fluctuations. Managing stress through rest, mindfulness, or professional help may help reduce symptom flare-ups and support overall wellbeing.
While diet cannot cure TED, maintaining balanced nutrition supports thyroid function and tissue healing. A diet rich in antioxidants, selenium, and omega-3 fatty acids can be beneficial. It is also advisable to limit salt and alcohol intake to reduce swelling and inflammation.
Contact lens wear can become uncomfortable during the active phase of TED due to dryness or eyelid swelling. Most patients prefer glasses until inflammation settles. Once the condition stabilises, contact lens use may be resumed under the guidance of an eye specialist.
Recurrence is uncommon but can happen, especially if thyroid hormone levels become unstable or if the patient resumes smoking. Regular follow-up appointments and maintaining optimal thyroid control help prevent relapse.
Simple lifestyle habits can make a difference—stop smoking, protect eyes from wind and sunlight with sunglasses, use lubricating drops, sleep with your head elevated, and maintain consistent thyroid treatment as advised by your endocrinologist.
Other blogs related to eye conditions
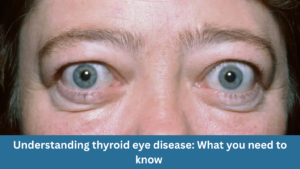
Understanding thyroid eye disease: What you need to know
Understanding thyroid eye disease: What you need to know At Clarity Eye Surgeons in Canberra, our team of skilled ophthalmologists in Canberra brings years of
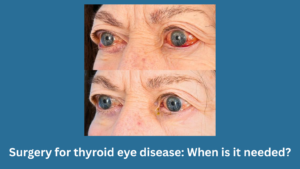
Surgery for thyroid eye disease: When is it needed?
Surgery for thyroid eye disease: When is it needed? At Clarity Eye Surgeons in Canberra, our team of experienced ophthalmologists, led by Dr Parth Shah,

Pterygium surgery: What to expect before, during, and after?
Pterygium surgery: What to expect before, during, and after? At Clarity Eye Surgeons in Canberra, patients receive expert care led by Dr Parth Shah, a

Living with thyroid eye disease: Treatment options explained
Living with thyroid eye disease: Treatment options explained At Clarity Eye Surgeons in Canberra, our team of highly qualified ophthalmologists has extensive experience diagnosing and
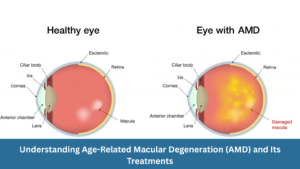
Understanding Age-Related Macular Degeneration (AMD) and Its Treatments
Understanding Age-Related Macular Degeneration (AMD) and Its Treatments At Clarity Eye Surgeons, we bring decades of ophthalmic expertise and advanced surgical experience to help Canberra

Diabetic eye disease: How to prevent vision loss?
Diabetic eye disease: How to prevent vision loss? What is diabetic eye disease? Diabetic eye disease refers to a group of eye conditions that can

Common vision problems in children and how to spot them early
Common vision problems in children and how to spot them early At Clarity Eye Surgeons in Canberra, our team of highly experienced paediatric ophthalmologists and

Double vision in children: What parents should know
Double vision in children: What parents should know Double vision, medically called diplopia, occurs when a child sees two images of a single object instead

Glaucoma: What it is, Symptoms, Causes, Types & Treatment
Glaucoma: What it is, Symptoms, Causes, Types & Treatment Glaucoma is often called the “silent thief of sight” because it can damage your vision gradually,

Living with wet macular degeneration: Treatment options and lifestyle tips
Living with wet macular degeneration: Treatment options and lifestyle tips Wet macular degeneration, also known as neovascular age-related macular degeneration (AMD), is a chronic eye

Retinal detachment: Early signs you should never ignore
Retinal detachment: Early signs you should never ignore Your eyes are extraordinary organs that allow you to experience the world in vivid colour, detail, and

Vitrectomy: What you need to know
Vitrectomy: What you need to know Vitrectomy is a specialised eye surgery performed to treat a range of disorders affecting the retina and vitreous —

Diabetes and your eyes: What you need to know
Diabetes and your eyes: What you need to know Diabetes is a chronic condition that affects how your body regulates blood sugar (glucose). While most

Nystagmus: Symptoms, Causes, and Treatments
Nystagmus: Symptoms, Causes, and Treatments Nystagmus is a condition in which the eyes make uncontrolled, repetitive movements. These movements can be slow or fast, side-to-side

What to know about blurry vision and diabetes?
What to know about blurry vision and diabetes? Blurry vision is a common and often early symptom of diabetes. If you or someone you know
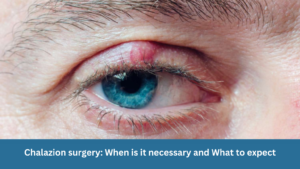
Chalazion surgery: When is it necessary and What to expect
Chalazion surgery: When is it necessary and What to expect A chalazion is a common eyelid condition that can lead to discomfort, swelling, and cosmetic

Are prescription glasses effective for treating lazy eye?
Are prescription glasses effective for treating lazy eye? Lazy eye, also known as amblyopia, is a common vision problem in children, affecting a small percentage

Dry Eye Syndrome: Symptoms, Causes & Treatment
Dry Eye Syndrome: Symptoms, Causes & Treatment Do your eyes often feel dry, irritated, or fatigued? You might be experiencing Dry Eye Syndrome (DES)—a common

The Relationship Between Allergies and Eye Health in Children
The Relationship Between Allergies and Eye Health in Children Allergies are a prevalent concern among children and can significantly impact their quality of life. While

Understanding Astigmatism: Symptoms, Causes, Diagnosis, Treatment Options & Prevention
Understanding Astigmatism: Symptoms, Causes, Diagnosis, Treatment Options & Prevention What is Astigmatism? Astigmatism is a common eye condition that affects how your eye focuses light.
Understanding Retinal Detachment: Causes, Symptoms, Diagnosis and Treatment
Understanding Retinal Detachment: Causes, Symptoms, Diagnosis and Treatment As the principal ophthalmologist at Clarity Eye Surgeons, Dr Parth Shah is passionate about educating our patients
