Table of Contents
ToggleHow intravitreal injections help preserve vision in diabetic retinopathy?

Dr Parth Shah, an experienced ophthalmologist at Clarity Eye Surgeons, specialises in the diagnosis and management of diabetic retinopathy and other complex retinal conditions. With advanced expertise in retinal imaging and intravitreal injection techniques, Dr Shah provides personalised, evidence-based care focused on preserving vision, preventing complications, and improving long-term eye health. His commitment to precision, transparency, and patient-centred care ensures that every individual receives the highest standard of treatment and ongoing support.
What are intravitreal injections?
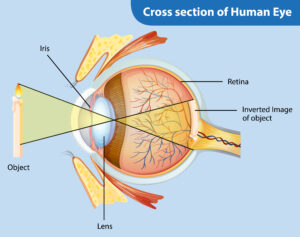
Intravitreal injections are specialised treatments delivered directly into the vitreous cavity of the eye. They allow medications to act immediately on the retina, controlling disease processes that can lead to vision loss. In diabetic retinopathy, these injections commonly use anti-VEGF (vascular endothelial growth factor) drugs or corticosteroids. Anti-VEGF medications block abnormal blood vessel growth, while corticosteroids reduce inflammation and fluid leakage, helping stabilise the retina.
How do intravitreal injections preserve vision?

These injections target the root causes of retinal damage in diabetic retinopathy. They reduce fluid leakage, minimise retinal swelling (macular oedema), and prevent abnormal blood vessel growth (neovascularisation). By doing so, intravitreal injections stop further deterioration of vision and lower the risk of severe complications such as vitreous haemorrhage or retinal detachment. Early treatment preserves existing vision and prevents irreversible damage.
Who can benefit from intravitreal injections?
Patients at risk of vision loss from diabetic retinopathy are the main beneficiaries. This includes individuals with:
- Macular oedema causes swelling in the central retina.
- Proliferative diabetic retinopathy with new, fragile blood vessels.
- Early retinal damage detected during routine eye exams.
Even patients with mild symptoms can benefit, as early intervention prevents future vision deterioration. Our ophthalmologists assess each patient individually to determine suitability for treatment.
How often are intravitreal injections required?
The frequency depends on disease severity and individual response:
- Initial treatment may involve monthly injections for 3–6 months.
- Maintenance injections may continue every 6–12 weeks based on retinal response.
- Regular monitoring with optical coherence tomography (OCT) ensures optimal timing and dosing.
Consistency is critical. Missing appointments can reduce effectiveness and increase risk of complications.
Are intravitreal injections safe?
When administered by trained retinal specialists, intravitreal injections are very safe. Most patients experience only minor side effects, including mild irritation, redness, or temporary blurred vision. Serious complications such as infection (endophthalmitis) are extremely rare and are managed immediately in specialised eye centres. At Clarity Eye Surgeons, strict aseptic protocols and advanced techniques minimise risks and ensure patient safety.
What results can patients expect?
Patients often experience:
- Reduced retinal swelling and improved macular function.
- Stabilisation or improvement of visual acuity.
- Slowed disease progression and reduced risk of severe vision loss.
While intravitreal injections are not a cure for diabetic retinopathy, they significantly improve long-term visual outcomes. Consistent treatment combined with blood sugar management maximises benefits.
How do you prepare for an intravitreal injection?
Preparation is simple:
- Eye drops are used to numb the eye for comfort.
- Pupils may be dilated for a brief examination before injection.
- Patients are advised to avoid rubbing their eyes and to follow post-injection care instructions.
The procedure is quick, typically taking 10–15 minutes, and patients can return home immediately after.
How long does it take to see improvement?
Some patients notice subtle vision improvement within a few weeks. Significant stabilisation of retinal swelling and improved visual outcomes may take months. Regular follow-up appointments allow ophthalmologists to track progress and adjust treatment schedules as necessary.
Why choose Clarity Eye Surgeons for intravitreal injections?
At Clarity Eye Surgeons, we combine:
- Advanced retinal imaging and diagnostics.
- Skilled ophthalmologists with decades of experience.
- Personalised treatment plans focused on safety and effectiveness.
- Patient education and support throughout the treatment process.
Our clinic prioritises both immediate and long-term vision preservation, ensuring that patients receive expert care at every stage of diabetic retinopathy.
Conclusion
Intravitreal injections are a highly effective, safe, and targeted treatment for preserving vision in diabetic retinopathy. By addressing retinal swelling, abnormal blood vessel growth, and inflammation, these injections help stabilise vision and prevent severe complications. Early intervention and consistent follow-up are key to achieving the best outcomes.
At Clarity Eye Surgeons, our experienced team combines advanced technology, personalised care, and proven expertise to ensure each patient receives the most effective treatment for their eyes. If you or a loved one is experiencing diabetic eye changes or vision concerns, book a consultation with Clarity Eye Surgeons today and take the first step towards preserving your vision.
Author Bio
Dr Parth Shah is a director and principal ophthalmologist at Clarity Eye Surgeons in Canberra, specialising in eye injections for retinal disease, cataract surgery & strabismus (eye muscle) surgery. With extensive training and experience, he is renowned for his expertise in the field. Dr Shah is dedicated not only to performing successful surgeries but also to patient education. His compassionate approach, combined with technical proficiency, has earned him the trust and gratitude of countless patients. He is a true advocate for eye health and a trusted name in the Canberra ophthalmology community.
FAQs
Intravitreal injections primarily stabilise vision and prevent further deterioration. While some patients may notice slight improvement, they cannot fully reverse existing retinal damage.
Most patients feel minimal discomfort. The eye is numbed with anaesthetic drops, and some may experience a brief pressure sensation during the injection.
Typically, only one eye is treated per session to minimise risk of complications. The second eye is treated in a separate appointment if required.
Patients are usually advised not to drive immediately after the procedure due to temporary blurring from anaesthetic or dilating drops. Most can drive once vision stabilises, usually the next day.
Patients should avoid rubbing the eye, swimming, or exposing the eye to unclean water for a few days. Normal daily activities can generally be resumed quickly
The duration varies depending on the medication used and individual response. Some injections last 4–6 weeks, while others may be effective for 8–12 weeks, requiring repeated treatments.
Yes, injections can be combined with laser therapy or surgery if needed. Your ophthalmologist will create a personalised treatment plan based on your retinal condition.
No, these injections act locally within the eye and do not influence systemic blood sugar levels.
Long-term risks are minimal when administered properly, but rare complications can include cataract formation or increased eye pressure. Regular monitoring helps manage these risks.
Other blogs related to Eye Conditions

Eye conditions in premature infants (e.g. ROP) — What parents should know
Eye conditions in premature infants (e.g. ROP) — What parents should know Premature infants face a range of medical challenges, and their eyes are no
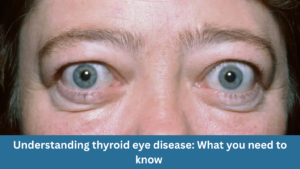
Understanding thyroid eye disease: What you need to know
Understanding thyroid eye disease: What you need to know At Clarity Eye Surgeons in Canberra, our team of skilled ophthalmologists in Canberra brings years of
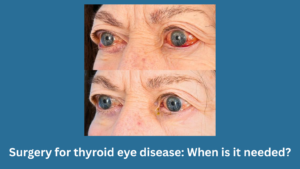
Surgery for thyroid eye disease: When is it needed?
Surgery for thyroid eye disease: When is it needed? At Clarity Eye Surgeons in Canberra, our team of experienced ophthalmologists, led by Dr Parth Shah,

Pterygium surgery: What to expect before, during, and after?
Pterygium surgery: What to expect before, during, and after? At Clarity Eye Surgeons in Canberra, patients receive expert care led by Dr Parth Shah, a

Living with thyroid eye disease: Treatment options explained
Living with thyroid eye disease: Treatment options explained At Clarity Eye Surgeons in Canberra, our team of highly qualified ophthalmologists has extensive experience diagnosing and
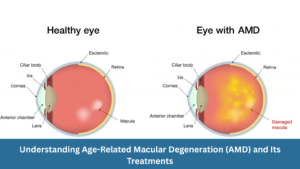
Understanding Age-Related Macular Degeneration (AMD) and Its Treatments
Understanding Age-Related Macular Degeneration (AMD) and Its Treatments At Clarity Eye Surgeons, we bring decades of ophthalmic expertise and advanced surgical experience to help Canberra

Diabetic eye disease: How to prevent vision loss?
Diabetic eye disease: How to prevent vision loss? What is diabetic eye disease? Diabetic eye disease refers to a group of eye conditions that can

Common vision problems in children and how to spot them early
Common vision problems in children and how to spot them early At Clarity Eye Surgeons in Canberra, our team of highly experienced paediatric ophthalmologists and

Double vision in children: What parents should know
Double vision in children: What parents should know Double vision, medically called diplopia, occurs when a child sees two images of a single object instead

Glaucoma: What it is, Symptoms, Causes, Types & Treatment
Glaucoma: What it is, Symptoms, Causes, Types & Treatment Glaucoma is often called the “silent thief of sight” because it can damage your vision gradually,

Living with wet macular degeneration: Treatment options and lifestyle tips
Living with wet macular degeneration: Treatment options and lifestyle tips Wet macular degeneration, also known as neovascular age-related macular degeneration (AMD), is a chronic eye

Retinal detachment: Early signs you should never ignore
Retinal detachment: Early signs you should never ignore Your eyes are extraordinary organs that allow you to experience the world in vivid colour, detail, and

Vitrectomy: What you need to know
Vitrectomy: What you need to know Vitrectomy is a specialised eye surgery performed to treat a range of disorders affecting the retina and vitreous —

Diabetes and your eyes: What you need to know
Diabetes and your eyes: What you need to know Diabetes is a chronic condition that affects how your body regulates blood sugar (glucose). While most

Nystagmus: Symptoms, Causes, and Treatments
Nystagmus: Symptoms, Causes, and Treatments Nystagmus is a condition in which the eyes make uncontrolled, repetitive movements. These movements can be slow or fast, side-to-side

What to know about blurry vision and diabetes?
What to know about blurry vision and diabetes? Blurry vision is a common and often early symptom of diabetes. If you or someone you know
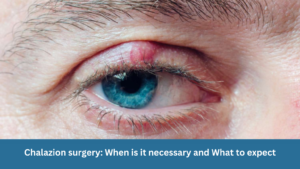
Chalazion surgery: When is it necessary and What to expect
Chalazion surgery: When is it necessary and What to expect A chalazion is a common eyelid condition that can lead to discomfort, swelling, and cosmetic

Are prescription glasses effective for treating lazy eye?
Are prescription glasses effective for treating lazy eye? Lazy eye, also known as amblyopia, is a common vision problem in children, affecting a small percentage

Dry Eye Syndrome: Symptoms, Causes & Treatment
Dry Eye Syndrome: Symptoms, Causes & Treatment Do your eyes often feel dry, irritated, or fatigued? You might be experiencing Dry Eye Syndrome (DES)—a common

The Relationship Between Allergies and Eye Health in Children
The Relationship Between Allergies and Eye Health in Children Allergies are a prevalent concern among children and can significantly impact their quality of life. While

Understanding Astigmatism: Symptoms, Causes, Diagnosis, Treatment Options & Prevention
Understanding Astigmatism: Symptoms, Causes, Diagnosis, Treatment Options & Prevention What is Astigmatism? Astigmatism is a common eye condition that affects how your eye focuses light.
Understanding Retinal Detachment: Causes, Symptoms, Diagnosis and Treatment
Understanding Retinal Detachment: Causes, Symptoms, Diagnosis and Treatment As the principal ophthalmologist at Clarity Eye Surgeons, Dr Parth Shah is passionate about educating our patients
